You arrive late for your doctor’s appointment because traffic was awful and your transportation provider was behind schedule. You’re anxious about being late and when the receptionist impatiently asks about your insurance coverage, you quickly fumble through your wallet to find your cards. She glances at the first card you hand her and says they don’t accept Medicaid. You’re worried you will be turned away when the receptionist points to a red, white, and blue insurance card in your hand and asks for your $20 copay. You don’t have $20 (and you’re pretty sure you shouldn’t have a copay but don’t want to say anything). You’re trying to remember the list of health concerns you wanted to share with the doctor. You’re confused. You’re frustrated. You’re one of the 12 million dual eligibles in this country.
Individuals dually eligible for Medicare and Medicaid are a medically and socially complex population, often with functional limitations and unmet behavioral health needs. And as the example above demonstrates, in many instances this population must navigate complex, misaligned, and fragmented health care and social service systems. This fragmentation can lead to stress for both the individual and their caregivers, poorer health outcomes, and individuals receiving incomplete care in inappropriate settings.
The Centers for Medicare and Medicaid Services (CMS) and states are making strides in addressing this system fragmentation through programs such as Medicare Advantage Dual Special Needs Plans (DSNPs). DSNP options are between Medicare and Medicaid, often based on the design of the Medicaid program in their state.
Example DSNP Program | Description |
Stand-Alone DSNP Coordinated with Medicaid Fee-for-Service (FFS) | Several states exclude dual eligibles from Medicaid managed care programs and many other states use FFS for all individuals served by Medicaid. In these markets, the higher-touch, targeted model of care DSNPs provide to dual eligibles can make a considerable difference in their well-being. Despite the lack of Medicaid managed care, DSNPs can help coordinate Medicaid services by providing dual eligibles with appropriate education and supports, including assistance related to Medicaid grievances and appeals. |
Stand-Alone DSNP Coordinated with Medicaid Managed Care | In states with Medicaid managed care for dual eligibles, different organizations may administer the Medicaid and Medicare benefit and the DSNP’s parent organization may not be contracted to provide Medicaid coverage. In these instances, the DSNP organization offers a targeted model of care and benefit design, and works with a separate Medicaid Managed Care Organization (MCO) to ensure a coordinated experience for a dual eligible. |
DSNP with Companion Medicaid Managed Care (HIDE SNP) | In 2020, CMS is implementing a new definition for DSNPs whose parent organization is also responsible for Medicaid behavioral health and/or long-term services and supports (LTSS) in the state, calling the plan a Highly Integrated DSNP (HIDE). HIDE SNPs provide coordination and targeted care models for all enrollees, and also allow for alignment between Medicare and Medicaid for duals enrolled with the organization for both sets of benefits. |
FIDE SNP | Fully Integrated DSNPs (FIDE SNPs) are possible in states with managed LTSS programs. A FIDE SNP must have a comprehensive Medicaid contract in the state that covers at least 180 days of nursing facility coverage per year, as well as special designation from both the state and CMS to be a FIDE SNP. Unlike other SNP types, some FIDE SNPs are eligible for a Medicare “frailty adjustment payment” to accommodate models responsive to the complex needs of an LTSS population. In addition to the value detailed in each DSNP program above, FIDE SNPs also have integrated member materials and processes, and can more comprehensively manage the needs of duals. |
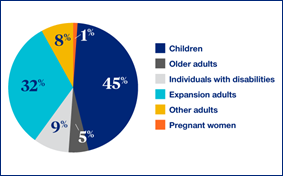
DSNP is one of many approaches that integrate Medicare and Medicaid for dual eligibles, with other approaches including the Financial Alignment Initiative and the Program of All-Inclusive Care for the Elderly (PACE). Each approach has strengths and limitations, but a key advantage of DSNP is the flexibility of the program. The broad array of DSNP options available to states makes it easier to implement than other dual programs.. Also, Congress permanently authorized DSNPs in 2018. This permanency allows for longer-term investment in establishing and administering the program by states and managed care organizations and coupled with state flexibility, allows states to evolve the program over time based on lessons learned and state readiness. Finally, DSNP is scalable. States can leverage the DSNP program to serve the entirety of the dual eligible population, including all ages as well as “full” and “partial” duals, while still building out distinct DSNP programs within a state to target sub-populations, such as those in need of LTSS.
The health policy environment surrounding dual eligibles is rapidly evolving as policy makers better understand the population and the fragmented maze of health care they are trying to navigate.
Read more from Allison Rizer