Covid-19 and long-term impacts to health care delivery
Since a public health emergency (PHE) was officially declared on January 31, 2020 and an official national emergency proclaimed on March 13, 2020, the global COVID-19 pandemic has impacted the lives of all Americans and dramatically shifted our way of living. In addition to the suffering that has been endured due to the loss of loved ones and economic hardships faced by millions of Americans, the health care system - and specifically the Medicaid program - has been significantly impacted. Included in this Addendum are details of how state budget pressures are playing a role in the impacts being felt in the Medicaid program, highlights of potentially long-term changes to the way care in Medicaid is delivered, and an overview of new partnership opportunities in Medicaid to help better support the individuals and communities it serves.
The trends included in this addendum are not the only impacts brought on by COVID-19 but are trends that may fundamentally shift the system.
Trend 1: State budgets & Medicaid funding
Prior to the start of the global pandemic, states had experienced nine consecutive years of spending and revenue growth. In 2020, that trend was reversed. The PHE significantly impacted both revenues and expenses in state budgets. On the revenue side, with many businesses having to close or significantly scale back operations, many states experienced a FY 20 decline in sales tax revenue, the largest source of state general revenue funding.1 Other revenue sources were also affected, declining between 3 and 17.5%.2 Alongside this decline in revenue, states needed to deploy additional resources to address COVID-19, such as the purchase of PPE, distribution of vaccines, or standing up new technologies to accommodate teleworking and virtual learning. Based on early estimates, these additional expenses could amount to almost $180B for states and counties through FY 21.3
This impact to revenues and expenses has meant that policymakers needed to make difficult decisions about where to allocate limited resources. In 2020, over 30 states reported using spending cuts due to revenue shortfalls to balance their budgets.4 Decisions were made regarding funding of critical items such as schools, jails/prisons and infrastructure, along with others against available funding and large obligations like federal Maintenance of Effort (MOE) requirements. States are currently drawing down an enhanced Federal Medical Assistance Percentage (FMAP) of 6.2% that has an associated MOE requirement. Receipt of these dollars will continue through the end of the quarter in which the PHE ends. On January 22, the then Acting Secretary of the Department of Health and Human Services Norris Cochran, sent a letter to the nation’s Governors indicating that in all likelihood the Secretary would continue to renew the PHE in 90-day increments through the end of 2021. Additionally, the Acting Secretary indicated that states will be given 60 days’ notice prior to the PHE ending. This provides states with some predictability around enhanced funding to support their Medicaid program and other federal funding streams that use the FMAP reimbursement structure. However, most state Medicaid directors have noted that the enhanced FMAP does not fully cover the cost of the increases in their Medicaid rolls due to the MOE requirement.5
The increased FMAP and Congressional funding have served as a critical lifeline for states experiencing revenue declines and large, unexpected expenses. This was made clear during recent state legislative sessions where budgets passed were up 10% or more in many states.6 When the PHE officially ends — ending the enhanced FMAP funding along with the MOE requirement — we should anticipate that COVID-19 will continue to have an impact on state budgets. In particular, though the current increase in Medicaid enrollments is attributed largely to the MOE requirement, given the economic impacts of the PHE, sustained increases in the number of individuals enrolled in Medicaid may be possible, but would need to be supported without the enhanced federal funding to offset those additional costs. Though it may ultimately not substantively impact the overall health of state budgets, it is an important factor to keep in mind and one that might drive states to additional budget actions. As a result, the full effect of the PHE may linger beyond its official end and potentially years into the future.
Trend 2: Health care delivery system
The COVID-19 pandemic severely strained the health care system and required front-line workers to take on more, both physically and mentally, to respond to the crisis as their colleagues quarantined, contracted COVID-19, or were unable to work due to being high-risk or having caretaker responsibilities at home. Each part of the health care system continues to face a unique set of issues that are likely to have effects beyond the pandemic, including:
- Hospitals: The American Hospital Association estimates that the pandemic cost U.S. hospitals and health systems $202.6 billion between March 1st and June 30th in 2020, due to decreased utilization, increased costs, and staffing challenges.7 Congress allocated COVID-19 relief funds to hospitals, but facilities with larger portions of privately insured patients and high pre-pandemic operating margins received a greater portion of those funds.8 This left rural hospitals and similar facilities with less access to this critical funding, due to their focus on serving Medicare and Medicaid populations and overall lower patient volume. These facilities entered the pandemic with already thin margins, workforce shortages, and challenging dynamics serving their communities due to geographic isolation.9 The added pressure from the pandemic has the potential to further increase consolidation or spur additional closures, leading to a decline in the number of rural hospitals and other similar facilities further exacerbating the issue of access to care for those populations they serve.
- Federally Qualified Health Centers (FQHCs): FQHCs serve over 30 million Americans, including 1 out of every 5 Medicaid members.10 The two leading challenges these providers reported facing prior to the pandemic were financial solvency and workforce shortages. Both were exacerbated by the pandemic due to revenue decreases, site closures (particularly dental and school-based clinics), and staffing challenges.11 Even with increased capacity due to expansion of telehealth, these challenges are likely to continue throughout 2021 as FQHCs work to balance the continued resource demands associated with COVID-19 testing, vaccine distribution, and on-going patient care. Communities served by FQHCs could experience access issues beyond the pandemic depending on the federal and state supports provided to FQHCs to help address these current and increasing challenges.
- Long-term care facilities: Nursing homes and other long-term care facility residents and staff have been disproportionally affected by COVID-19. Nationally, 6% of all cases and 38% of deaths from the virus are associated with long-term care settings.12 While this created greater demand for in-home care services, the pent-up demand for rehabilitation services along with the aging U.S. population continue to drive demand for facility-based services. Prior to the pandemic, facilities faced workforce shortages due to low wages and limited benefits. Those shortages have been compounded by the pandemic as long-term care facilities continue to lose staff (7.8% of employees since February 2020) even as overall health care employment rebounds.13
Trend 3: Health at home
The COVID-19 PHE changed the landscape of health care delivery and utilization in many ways. From the beginning of the pandemic, individuals were encouraged to stay at home; both to minimize risk of disease exposure and to ensure that vital health care resources remained available for individuals battling COVID-19. This initially led to a decrease in preventive and elective health care services, ambulatory care utilization and hospital admissions.14 The shift in care delivery presented an opportunity to leverage existing capabilities and innovative technology to deliver health care to individuals at home. Additionally, the disproportionate impact of COVID-19 on nursing homes highlighted the vulnerability of individuals living and working in congregate, institutional settings and put renewed focus on long-term care delivery. States were able to leverage emergency flexibilities to support existing Home and Community-Based Services (HCBS) and long-term services and supports (LTSS) infrastructure and increase access to telehealth.15 After the PHE ends, state and federal policymakers need to assess which, if any, of the changes should be permanently adopted.
Flexibilities allowed during PHE
HCBS waiver flexibility
As of March 2021, all 50 states and the District of Columbia had at least one 1915 (c) Appendix K waiver approved by CMS.16 An Appendix K is a standalone appendix used to amend a specific waiver, multiple approved waivers, or all approved waivers in a state. CMS created a specific Appendix K template for the COVID-19 PHE to help states quickly identify available flexibilities and streamline the approval process. The template gave states the option to modify policies related to access and eligibility, expand covered services, and support financial stability for existing HCBS workforce via retainer payments.
Provider and service delivery flexibility
With a greater number of individuals needing health care delivered at home, states looked for opportunities to leverage existing family caregivers, flex providers where they were most needed, and support the already stretched HCBS workforce. Once the PHE was declared, states were able to submit Section 1135 waivers to amend certain requirements related to Medicare, Medicaid, and the State Children’s Health Insurance Program (CHIP). CMS also released a template for State Plan Amendments (SPAs) to address changes related to the PHE. These tools gave states the opportunity to adapt provider requirements in a variety of ways to rapidly improve access to health care at home. All 50 states plus the District of Columbia leveraged Section 1135 waivers to allow out-ofstate providers with equivalent licensing in another state to provide care. Some states expanded the workforce by allowing family members or member representatives to deliver personal care services. Other states sought to increase the payment rate for personal care attendants or expand the provider types that can order, certify, and recertify member’s home health care plans.17 Equally important as expanding the pool of providers was allowing reimbursement for services delivered in the home. For example, 30 states used Section 1135 waivers to allow HCBS services to be delivered in settings that did not meet traditional HCBS settings criteria.
Telehealth
Telehealth is one of the key tools leveraged during the PHE to address health care needs. CMS released a State Medicaid & CHIP Telehealth Toolkit in April of 2020, which identified key areas of telehealth for state consideration.18 Flexibilities included allowing traditional telephone calls as qualifying technological modalities, expanding the originating sites (patient location) eligible to utilize telehealth, adjusting payment rates for services, and expanding the types of services allowed to be delivered via telehealth.
Flexibilities allowed post-PHE
As part of post-PHE program design conversations, there is already a focus on allowing, in some capacity, the continued expansion of covered telehealth benefits and flexibilities leveraging HCBS. Additional research is warranted to ensure delivery of high-quality care and safeguards against fraud, waste, and abuse.
Trend 4: Role of public health in health care
Public health funding has faced funding cuts at the state and local level by 16% and 18% respectively since 2010.19 As a result of these continued cuts, health departments have dealt with reduced capacity and availability of resources, including a diminished workforce, which were then exacerbated by additional budget and resource constraints due to the COVID-19 pandemic. These underlying challenges within the public health support system and infrastructure contributed to the nation’s initially limited ability to respond effectively to the global pandemic. In order to effectively address ongoing and emerging public health threats, the capacity shortages magnified by the COVID-19 pandemic will need to be addressed. The health care system can be a partner in supporting many of these efforts.
Public health funding & workforce
Prior to the COVID-19 pandemic, the public health workforce was dwindling, due in part to funding cuts, but also due to the fatigue that funding cuts placed on the workforce.20 Over 38,000 jobs have been lost in state and local public health departments since 2008, resulting in a depreciated workforce and a limited ability to focus on regular duties such as chronic disease control, mental health surveillance, and routine vaccination administration.
The public health workforce is also notably aging, as it has been unable to lure young professionals due in large part to the budget constraints that limit wage levels and benefits. The PHE has exacerbated ongoing capacity and fatigue issues among the public health workforce. Additional budget cuts pose the threat of more or longer layoffs, further aggravating workforce capacity and fatigue concerns. Ultimately, public health departments have been asked to take on more responsibilities, all while having their funding reduced.

Critical role of public health
The public health system provides a number of critical services that have been impacted by the COVID-19 pandemic, two of which are described here:
Routine vaccines
Childhood vaccination rates plummeted across the U.S. as a result of the PHE and resulting stay-at-home orders. Even as stay-athome orders are lifted or relaxed, vaccination rates still lag, likely due to parental concerns about exposing their child to COVID-19 during a well-child visit. These children are at risk for contracting dangerous diseases such as measles or pertussis (whooping cough) if they are not vaccinated before they begin to return to preschool, school, or daycare. In addition, flu vaccination rates for adults in the U.S. are traditionally low. While flu vaccine rates have increased over the last decade, only 48.4% of adults 18 and older received the flu vaccine in 2019-20.21 If childhood vaccination rates do not return to pre-COVID levels and adult vaccination rates remain low, the U.S. risks the resurgence of preventable diseases and future disease outbreaks.
Mental health
While not often seen as a public health issue, negative mental health is a leading cause of disease in the U.S. and impacts a significant portion of the U.S. population. In 2019, 20.6% of all U.S. adults, or 51.5 million, suffer from any mental illness (AMI).22 Reports related to substance use overdoses and domestic violence incidents have increased during the pandemic, as have calls to mental health and suicide hotlines. The Centers for Disease Control and Prevention (CDC) estimates that the number of adults with symptoms of anxiety disorder and/or depressive disorder has quadrupled since the beginning of the pandemic.23
There are several contributing factors related to the rise in mental health related incidences. The COVID-19 pandemic has negatively impacted social determinants of health (SDOH) such as employment, food security, and homelessness, which often coincide with negative mental health experiences. In addition, the already fragmented availability of mental health providers has been exacerbated by the pandemic.
To combat the impact COVID-19 has had on mental health, the public health and health care systems need to work together and support state actions that:
- Expand telehealth infrastructure, capabilities, and coverage.
- Increase access to mental health providers, specifically targeting areas with provider shortages.
- Improve mental health disease surveillance.
Trend 5: Defining quality
The COVID-19 pandemic resulted in quality disruptions for both the 2019 and 2020 measurement years. For the 2019 measurement year, stay-at-home orders and social distancing guidelines disrupted health plan and provider performance evaluation activities, which would have occurred through onsite reviews during the spring of 2020. For the 2020 measurement year, there was a significant drop in health care utilization across the country, impacting health plan and provider performance against 2020 performance metrics, which were set prior to the start of the pandemic. As a result, states and the federal government took actions related to quality performance and evaluation given the impact of COVID-19, with long-term shifts in quality measurement possible in the coming years.
State and federal activity
Both at the federal level via the Centers for Medicare & Medicaid Services (CMS), and at the state level, there was a variety of guidance released in response to the inability to perform onsite reviews for the 2019 performance year. This guidance included:
- Early release of 2019 quality incentive pool funds,
- CMS encouragement of Medicaid and CHIP programs to utilize data collection methods for the 2019 measurement year that do not require in-person reviews, and
- Allowing managed care organizations (MCOs) contracted with certain Medicaid programs (e.g., Florida, California) to report their audited HEDIS 2019 hybrid rate if it was better than their HEDIS 2020 hybrid rate due to low chart retrieval
States and the federal government continue to evaluate the impact of the COVID-19 pandemic and its likely long-term impacts on quality measurement. Several states have adjusted their quality programs to include the impact of COVID-19. For example, Nevada preemptively suspended their quality program for 2021 and has not yet decided how the 2020 or 2021 measurement years will be used. In addition, Ohio shifted quality withholds from HEDIS measures to COVID-related criteria that managed care organizations (MCOs) must address collaboratively. This shift continued into 2021 and is focusing on two key areas: 1) childhood immunizations and lead testing and 2) improving diabetes A1c control.
Adjusting for the increased use of telehealth
In addition to the state and federal activities outlined above, the National Committee for Quality Assurance (NCQA) adjusted 40 quality metrics to account for the increased use and promotion of telehealth.24 It is unclear if NCQA intends these adjustments to be temporary during the PHE or if they will be permanent. Examples of adjustments include:
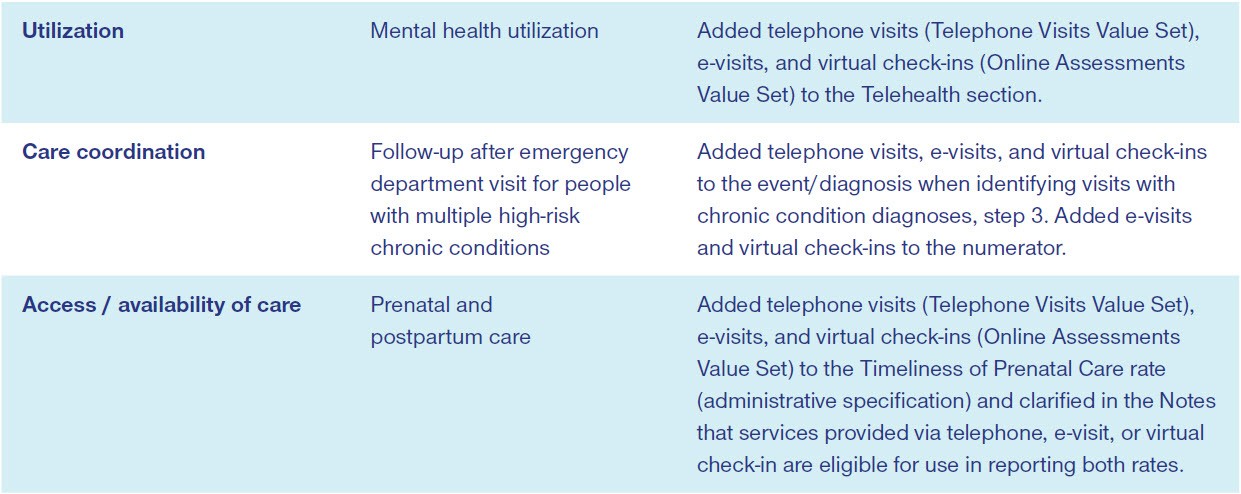
As telehealth continues to be leveraged as a vehicle for health care delivery during the COVID-19 pandemic, other quality measures are likely to be evaluated and adjusted to account for and include telehealth.
Shift in quality measurement
As quality metrics continue to be reviewed and altered due to the effects of COVID-19, there is an opportunity to shift how quality is measured to better incorporate related measures on activities to address health equity and social determinants of health (SDOH) such as housing, transportation, and nutrition. Several states, such as Michigan, are already exploring how to use innovative payment models to promote health equity through incentives.25 It is likely many others will begin evaluating how to incentivize MCOs and providers to produce equitable health outcomes for all populations.
Related content
Sources
- Center on Budget Priorities Opens in a new window
- National Association of State Budget Officers Opens in a new window
- Economy.com; National Association of Counties Opens in a new window
- National Association of State Budget Officers Opens in a new window
- Kaiser Family Foundation Opens in a new window
- Pew Opens in a new window
- Health Affairs Opens in a new window
- Kaiser Family Foundation Opens in a new window
- American Hospital Association Opens in a new window
- National Association of Community Health Centers Opens in a new window
- Kaiser Family Foundation Opens in a new window
- Kaiser Family Foundation Opens in a new window
- Altarum Opens in a new window
- Commonwealth Fund Opens in a new window
- Kaiser Family Foundation Opens in a new window
- Kaiser Family Foundation Opens in a new window
- Kaiser Family Foundation Opens in a new window
- CMS Opens in a new window
- Kaiser Health News Opens in a new window
- Kaiser Health News Opens in a new window
- Centers for Disease Control and Prevention Opens in a new window
- National Institute of Mental Health Opens in a new window
- Centers for Disease Control and Prevention Opens in a new window
- National Committee for Quality Assurance Opens in a new window
- National Committee for Quality Assurance Opens in a new window

