To serve the whole person, policymakers are advancing policy and program design initiatives that are focused on both access and care coverage and increasingly through the lens of equity. Using the authority granted in the Affordable Care Act (ACA) to expand Medicaid to individuals earning up to 138% of the federal poverty level (FPL) continues as a trend. In addition, access to not only physical and behavioral health services but also non-clinical services continue to be areas where states in particular are refocusing the approach to creating access to those services. Finally, spotlighted by the COVID-19 pandemic, health disparities and inequities in health care outcomes are being prioritized by federal and state policymakers through various actions, including new policies, additional procurement requirements, and new contract obligations.
Trend 3: Medicaid Expansion
In total, 38 states plus Washington, DC have adopted Medicaid Expansion.39 In just the last year, Idaho, Nebraska, and Utah have implemented Medicaid Expansion (after successful adoption in 2019) and two additional states, Missouri and Oklahoma, saw ballot initiatives pass for Expansion in 2020.40
States with previous or current movement and the potential opportunity to expand Medicaid in the next few years include:
- Florida: Advocates attempted to get Expansion on the ballot in 2020 but the Legislature made changes to the ballot process that thwarted their efforts. Advocates restarted their efforts in 2021 and signatures are being collected in order to secure a ballot measure in the 2022 election cycle.
- Mississippi and South Dakota both have signature drive efforts underway to put Expansion on the 2022 ballot. Though the effort continues in South Dakota, advocates in Mississippi paused their effort due to a state Supreme Court ruling that broadly effects all voter-based ballot initiatives.
- The Wyoming House successfully passed legislation that was ultimately rejected by the Senate. However, the Legislature’s Joint Revenue Committee revived the proposal setting it up for debate during an upcoming session.
- In Kansas, North Carolina, Wisconsin41, there has been movement to expand Medicaid, but efforts have run into partisan disagreements that appear insurmountable in the current environment.
- The Georgia legislature enacted legislation allowing the state to seek an 1115 waiver to expand Medicaid in 2019, which the State subsequently submitted and received approval of allowing expansion of Medicaid coverage to individuals earning up to 100% FPL (versus 138% as outlined in the ACA). Though implementation was set to begin July 1, 2021, the effort has been delayed due to push back from the Biden administration.42
- There have been no substantive efforts to date to expand Medicaid in Alabama, South Carolina, Tennessee, or Texas.
A total of six states have adopted Medicaid Expansion by ballot initiative that are considered ‘red’ or conservative (Idaho, Maine, Missouri, Nebraska, Oklahoma, and Utah).43 The use of ballot initiatives continues to be a trend with advocates using them in a number of the states that have yet to adopt Expansion. However, the Missouri legislature’s efforts to block implementation of Medicaid Expansion may serve as a new type of roadblock used in other states to delay or wholly prevent efforts to expand Medicaid.44 Though there has also been a trend in states tying Expansion coverage to meeting specific community engagement requirements, with the underlying authority for community engagement requirements in Medicaid anticipated to be withdrawn, this trend will likely end. If that occurs, it could have potential implications for states who were considering Expansion but only if they were able to tie the coverage to these requirements.

Trend 4: Addressing the Social Drivers of Health
Social drivers of health (SDOH) — social, economic, and environmental factors — continue to be primary drivers for health outcomes, health care costs, and quality. The latest estimate attributes approximately 80% of health outcomes to SDOH, including the following domains: housing, nutrition, transportation, employment, and interpersonal violence.45 The COVID-19 pandemic and accompanying economic impacts have compounded the negative impacts of SDOH, especially for the Medicaid population. Increasing state budget pressures continue to drive interest in addressing the negative impacts of SDOH that significantly impact health care costs.
Impact of COVID-19
COVID-19 has exacerbated the negative impacts of all SDOH domains, especially for Medicaid beneficiaries, and will likely last years beyond the pandemic. As of April 2021, key COVID-19 related impacts prevalent in the Medicaid community included:
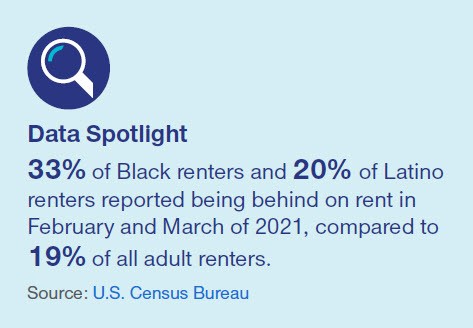
Housing: Prior to the pandemic, an average of 3.6 million eviction cases were filed annually in the U.S., but it estimated that the lifting of eviction moratoriums will put an estimated 30-40 million Americans at risk of eviction.46 This will likely continue the rise in homelessness seen in recent years—a study by the Economic Roundtable estimates homelessness, which sat just under 100,000 pre-pandemic recession, will climb 49% over the next four years, peaking in 2023.47
Nutrition: Food insecurity has increased across all states during the COVID-19 pandemic. State rates vary, ranging from 9.7% (North Dakota) to 22.6% (Mississippi) in 2020. Child food insecurity has risen as well, ranging from 15.0% (North Dakota) to 32.3% (Louisiana and Nevada), due in part to increased rates of poverty, but also to the shift from in-person to virtual learning, as low-income children rely heavily on free or reduced-price lunch at school for their primary source of food.48 Supplemental Nutrition Assistance Program (SNAP) enrollment has increased as a result.
Employment: The unemployment rate rose due to the economic downturn from the COVID-19 pandemic, hitting an alltime high in April 2020 (14.7%). Unemployment has since leveled off (measured 6.2% as of March 5) but remains elevated compared to pre-pandemic times (4.4% in March 2020). Low-wage jobs have been hit the hardest by the pandemic, accounting for 53% of jobs lost from February to November.49 At the beginning of the pandemic, temporary layoffs, also commonly referred to as “furloughs,” increased by over 15 million persons from March to April 2020 to hit 18.1 million persons total, while permanent job losses increased by 544,000 during that same time period. Since then, temporary layoffs have leveled off, accounting for 2.7 million unemployed persons in January 2021, while permanent job losses totaled 3.5 million in January 2021.
The COVID-19 pandemic has heightened the importance of addressing SDOH, increasing the appeal of new value-added services such as food assistance and home delivered meals, personal protective equipment, and pharmacy home deliveries. In total, 27 states reported implementing, expanding, or reforming a program or initiative in response to COVID-19 to address SDOH for Medicaid beneficiaries50. To respond to the increase in food insecurity due to COVID-19, states are using the SNAP flexibilities made available through the Families First Coronavirus Response Act (FFCRA) to provide emergency benefit supplements and reduce administrative procedures required to receive benefits.
Federal activity continues to address the COVID-19 impact on SDOH. President Biden signed an Executive Order to expand benefits for low-income families with children to account for meals missed due to COVID-related school and childcare closures. The American Rescue Plan Act includes $26 billion in rental assistance and $5 billion in assistance for individuals experiencing homelessness.51
Use of procurements, MCO contracts, & waivers
State Medicaid programs are increasingly prioritizing SDOH and their effects on health outcomes. States continue to use Medicaid managed care procurements and contracts to push MCOs to develop innovative solutions to address SDOH. In 2020, 35 states (out of 41 total managed care states) used contracts to promote addressing SDOH within the Medicaid program.52
The two most prevalent SDOH-related contractual requirements are social service referrals (31 states) and social needs screening (31 states). Social needs screening allows MCOs and providers to capture priority SDOH elements, which can help improve SDOH data. Improving accessibility of this data, even at an aggregate level, allows states to better coordinate programs and linkages across an individual’s whole life experience. States are also showing the increased desire to close referral loops through outcome tracking. The progression of SDOH contractual requirements in the last several years began with screening, evolved to include referrals, and are now expanding to include referral loop closure to ensure that social needs are not only identified, but also addressed.
As states place a greater emphasis on closing referral gaps and improving SDOH outcomes, interoperability between data systems and programs continues to grow in appeal, especially alignment at the Health Information Exchange (HIE) level. The increasing use of consistent and accessible data platforms has allowed for the possibility to connect information across all social risk points to better see the entire timeline of an individual.
State Medicaid programs are limited in how they can use federal funding to pay for social services, and as a result, states are finding innovative ways to utilize 1115 demonstration waivers to support SDOH initiatives. Several states have created funding streams through new or existing 1115 waivers including for tenancy supports (HI, MN, WA) and community-based organization direct payments (NC).
Partnerships & collaboration
Collaboration with community partners is increasingly important in the effort to address and solve for gaps in SDOH. States are encouraging MCOs to invest in collaborations with and between community-based organizations. Specific 2020 procurements that targeted collaboration include:
- Ohio: Required MCOs to commit a portion of profits to community re-investments that align with their population health strategy to target SDOH. Procurement criteria emphasized collaborative, community informed, and data-driven initiatives.
- Oklahoma: Required MCOs to partner with community-based organizations or social service providers and report on referrals to specific partners.
Even as more states place greater emphasis on closing referral gaps, community capacity is unlikely to meet the demand.
Trend 5: Health disparities and inequities
Health disparities, which are defined as a difference in health status that can be linked to social, economic, and/or environmental disadvantages53 are not a new phenomenon. Driven by longstanding realities in addition to deep roots in U.S. history, traditionally underserved racial and ethnic minority populations continue to be significantly impacted. And while communities struggle to overcome existing challenges, individual, provider, health system, societal, and environmental factors are creating new and widening disparities that need to be addressed.54 This deeply rooted societal challenge is clearer and more urgent today than ever as minority and other vulnerable populations are disproportionately affected by COVID-19.
Eliminating health disparities would result in a substantial reduction in health care costs, both directly ($230 billion) and indirectly ($1 trillion)55, demonstrating the additional impact that a focus on health equity can achieve. In addition, states are continuing to explore leveraging payment models to incentivize providers to promote health equity and reduce and eliminate health disparities.
State and federal activity
Compared to commercial and employer-based insurances, Medicaid covers a high proportion of underserved groups, meaning Medicaid beneficiaries are more likely to be impacted by health disparities. In 2019, racial and ethnic minorities comprised 58.9% of Medicaid beneficiaries.56 This has incentivized both the federal government and state Medicaid programs to place an emphasis on reducing health disparities, including the addition of a health disparities component to CMS quality initiatives.57 Several states, including Nevada, have also begun requiring MCOs to submit annual cultural competency plans to measure progress against health equity goals. The Nevada legislature also encouraged MCOs to align provider networks to meet the diversity of their Medicaid population, a trend likely to emerge nationally in the years to come.
States are increasingly using Medicaid managed care procurements and contractual requirements to target population health and address health disparities for Medicaid populations, with increasing focus on how managed care organizations are addressing disparities and structural racism within their own companies and systems. Most recently this has included:
Kentucky
- Applicants required to provide a detailed plan of how they planned to reduce or eliminate health disparities, including identifying partnerships, using innovative solutions, and data-sharing with providers.
Minnesota
- RFP included questions around managed care organizations’ antiracist systems and processes, both where they stand today and how organizations plan to improve upon them.
- Awardees will be required to report on specific initiatives that make a meaningful impact on disparities and health equity.
Ohio
- Required MCOs to employ a Health Equity Director within their organization.
- Required MCOs to promote and support the use of telehealth services to increase access and health equity across the state.
- Required MCOs to integrate health equity efforts into their population health strategy, information and technology infrastructure, and staffing.
- Required MCOs to collaborate with each other for a collective impact at reducing health disparities and improving population health.
Oklahoma
- Required applicants to provide an example of an innovative approach they have used to target health disparities and how this approach could be tailored to Oklahoma.
- Required applicants to identify and address how they will specifically target perinatal health disparities.
- Awardees will be required to use quality and outcome data to target and improve health disparities.
- Awardees will be required to participate in the Oklahoma Health Care Authority (OHCA) led effort to reduce health disparities.
- Awardees will be required to specifically target Tribal health disparities.
Pennsylvania
- Required MCOs to describe specific policies, procedures, and initiatives implemented to promote health equity in RFPs.
Given the magnification of health disparities by the COVID-19 pandemic, outlined below, it is expected that states will also look to leverage payment models that incentivize providers and MCOs to promote health equity.
Impact of COVID-19
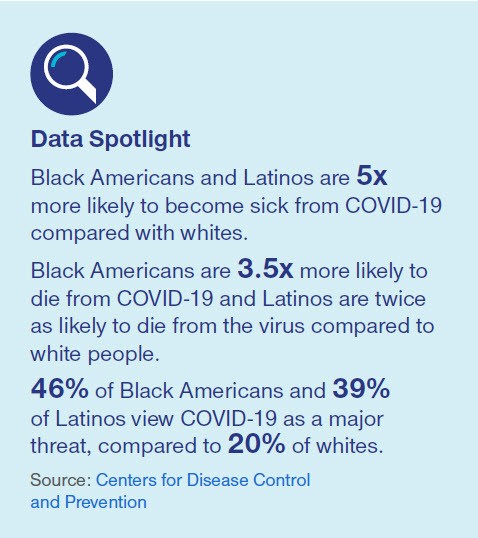
The COVID-19 pandemic has disproportionately affected underserved groups of society, including racial and ethnic minorities, rural populations, and socioeconomically disadvantaged populations, resulting in higher infection rates, hospitalization rates, and death rates. Contributors to this disproportionate impact include:
Occupation: For many in minority communities, adequate social distancing is not possible. Many are considered “essential” in industries such as food processing, manufacturing, transportation and service industry, leading to higher spread given the dynamics of their working environments, e.g. indoors, inability to telecommute. Additionally, given the work hours and lack of benefits typically associated with these occupations, essential workers often delay accessing treatment given an inability to take off work due to lack of sick time/paid time off or fear of losing their job.
Housing: Higher percentages of minority groups live in multigenerational households58, with many underserved individuals also experiencing crowded living conditions. Both factors can lead to increased risk of transmission and hinder COVID-19 prevention strategies. Further, people who are homeless – who suffer disproportionately from chronic illnesses – are largely unable to maintain social distancing.
Access: Health care costs and the lack of insurance often creates a barrier for underserved groups to seek care and treatment. Additionally, minority groups are often provided with different levels of care than their white counterparts. For example, among diabetes patients, Black Americans are less likely to receive influenza vaccinations, have glycosylated hemoglobin (HbA1c) testing or cholesterol testing.59 The delay of care can exacerbate conditions and put individuals at a higher risk of serious and/or fatal effects.
Systemic racism: Even after removal of long-standing rules and policies targeted at populations of color, the impacts continue to reverberate across society. A prominent example is the redlining of Black neighborhoods, which enabled the ability to ‘disinvest’ in the infrastructure and health of these communities. To this day, neighborhoods with historical ‘redlines’ see higher rates of pre-term births, cancer and mental illness.60
Distrust: Due to historic and persistent systemic racism and mistreatment, underserved groups often have a deep distrust of government and health care systems. The distrust continues to compromise numerous public health efforts, such as vaccine promotion and acceptance, and broadly creates hesitation to seek care.
Partnerships and collaboration
For Medicaid and managed care organizations, the instilled distrust of government and health care systems makes disparities and health equity an especially difficult trend to tackle. Addressing health disparities cannot happen within siloes; they must be approached in close collaboration and partnership with local leaders, community organizations, members, and providers. Any initiative aimed at addressing health disparities must include thoughtfully and culturally appropriate engagement designed to address the underlying causes. Ensuring that trusted community partners and providers are positioned as key leaders, and supported in their efforts, is critical in order to have meaningful, lasting impacts.
Related content
Sources
- CMS Opens in a new window
- Ibid
- CMS Opens in a new window
- Health System Tracker Opens in a new window
- Revcycle Intelligence Opens in a new window
- Kaiser Family Foundation Opens in a new window
- Kaiser Family Foundation Opens in a new window
- Kaiser Family Foundation Opens in a new window
- Medicaid.gov Opens in a new window
- Kaiser Family Foundation Opens in a new window
- Kaiser Family Foundation; The Commonwealth Fund Opens in a new window
- AHIP; Health Management Associates Opens in a new window
- Commonwealth Fund Opens in a new window
- MACPAC five states studied were: MN, NM, NY, OH, SC Opens in a new window
- Medicaid.gov Opens in a new window
- NPR Opens in a new window
- Kaiser Family Foundation Opens in a new window
- Michigan.gov Opens in a new window
- Health Affairs Opens in a new window
- Downside risk APMs are included as Categories 3B and 4A, 4B, and 4C in the HCPLAN Framework. Opens in a new window
- Bundled payment APMs are included as Category 3B in the HCPLAN Framework. Opens in a new window
- American Medical Association Opens in a new window
- mHealth Intelligence; Center for Connected Health Policy Opens in a new window
- MACPAC Opens in a new window
- Commonwealth Fund Opens in a new window
- Medicaid.gov Opens in a new window
- Commonwealth Fund Opens in a new window
- Commonwealth Fund Opens in a new window
- Commonwealth Fund Opens in a new window
- Medicaid.gov Opens in a new window
- Journal of the Academy of Nutrition and Dietetics Opens in a new window
- Medicaid.gov Opens in a new window
- Federal Communications Commission Opens in a new window
- Pew Research Opens in a new window
- Robert Woods Johnson Foundation Opens in a new window
- National Governors Association Opens in a new window
- Robert Woods Johnson Foundation Opens in a new window
- Health Affairs Opens in a new window
- Kaiser Family Foundation Opens in a new window
- Despite successful passage of the ballot measure, Missouri legislature is currently advancing a budget that does not fund the Expansion setting up a potential lawsuit.
- Wisconsin is unique as it has a modified Expansion coverage today.
- HealthInsurance.org Opens in a new window
- Bloomberg Law Opens in a new window
- As of the timing of this publication, the Missouri State Supreme Court has ruled that the state legislature did not need to allocate funding in order to for the state to move forward with implementing Medicaid Expansion as approved by the voters.
- Robert Wood Johnson Foundation Opens in a new window
- Aspen Institute Opens in a new window
- Economic Roundtable Opens in a new window
- Feeding America Opens in a new window
- Center on Budget and Policy Priorities Opens in a new window
- Kaiser Family Foundation Opens in a new window
- Center on Budget and Policy Priorities Opens in a new window
- Kaiser Family Foundation Opens in a new window
- Healthy People.gov Opens in a new window
- Kaiser Family Foundation Opens in a new window
- Association of State and Territorial Health Officials Opens in a new window
- Kaiser Family Foundation Opens in a new window
- Medicaid.gov Opens in a new window
- Pew Research Opens in a new window
- NCBI Opens in a new window
- New England Journal of Medicine Opens in a new window

